Friday, February 29, 2008
Saw a bird perching on the swing
It twisted and shrivelled into nothing
Then the ashes flew up
There was someone in my head
(His name is Sam)
And he told me to fly too
I like Sam for he is good to me
So I tried to fly but I couldn’t so I climbed
Up to the very top of the swing
Sam was angry because I hadn’t obeyed him exactly
He told me to jump or I would stop being a
Heroine from a fairytale
So I did
I hit the ground and it felt as if something
Had stabbed me all over though I couldn’t see any knives
I realised the all-important truth: the teacher had the knife
I cried buckets.
There is something about freedom
Which I will see soon
To Evelyn
Ever since I found out that Evangeline and Esther are down with schizophrenia, I feel very much indebted to my eldest daughter, Evelyn. Even though I have tried very hard all these years to be a responsible mother, I seem to have neglected Evelyn in many ways. All my attentions were on the twins.
Being always filial and understanding, Evelyn never complained. But deep down I know she does need my care and concern as much as Evangeline and Esther do. Evelyn, Mum hope you can really forgive me and understand that despite the fact I have put in more time to look after her sisters, Mum love you just as much.
Thursday, February 28, 2008
A Brief Introduction To Schizophrenia -- Treatment
There are two main aspects in the treatment of schizophrenia, namely medication and psychosocial treatment.
Medication
In the treatment of schizophrenia, there are different therapeutic options:
Ÿ Older, so called conventional antipsychotics
Ÿ Newer, so called atypical oral antipsychotics
Ÿ Long-acting atypical medication
Consistent taking of medication can allow a person with schizophrenia to lead a relatively normal life.
However, many patients with schizophrenia do not take their medication regularly. By taking a pause in the treatment the schizophrenia symptoms can come back. Research has shown that about 75% of people with schizophrenia relapse within a year to 18 months if antipsychotic drug therapy is stopped or taken inconsistently. Relapses are to be avoided, as they will lead to a new confrontation with the disorder, a further loss of social contacts and likely it will get worse every time.
Side effects of antipsychotic medication
Like virtually all medications, antipsychotics are not always free of unwanted effects along with their beneficial effects. Drowsiness, restlessness, muscle spasms, weight gain, tremor, dry mouth or blurring of vision are not unusual in the early phases of drug treatment. Most of these can be corrected by lowering the dosage or can be reduced by switching to another medication. Different patients respond differently to treatment and experience different side effects when taking antipsychotic drugs.
Psychosocial treatment
Medication alone is not a treatment. Schizophrenia patients often find it difficult to find or hold on to a job. Psychosocial support allows patients to build up social contacts, motivation or daily care. It generally focus on improving social functioning, be it in the hospital or in the community, at home or at work.
Ÿ Rehabilitation: rehabilitation programs focus on social and occupational training. Programs may include help in improving job skills, money management skills, use of public transport, social skills or problem solving skills. These training programs are especially important in a community-centered approach, supporting schizophrenia patients to lead their lives outside the hospital.
Ÿ Individual psychotherapy: In psychotherapy you have regular talks with your physician, psychologist or social worker. The sessions may focus on current or past problems, experiences, thoughts, feelings, or relationships. By sharing experiences with a person who has knowledge about schizophrenia, you may gradually gain a better insight in your situation and your mental problem. You will probably also feel supported, which can encourage you to overcome the difficult aspects of your condition. Family intervention: It is very important for caregivers to learn all they can about schizophrenia and its particular problems. For families experiencing difficulties in coping with the disease, family “psycho-education” may be an advisable solution. In this type of education caregivers are thought various coping strategies and problem-solving skills. This may help families deal more effectively with the condition of their relative.
Reference
Janssen Pharmaceutica, NV - Turnhoutseweg 30, 2340 Beerse, Turnhout RPR nr.0403.834.160 © Janssen Pharmaceutica, NV 2008 Last updated on 26 Jul 2007 http://www.janssen-cilag.com/
Lessons are so boring! The teacher just rattles off about things that I don't understand. I slept during most of the lessons or just stare blankly into space. I told mum that I don't want to go school but she says that it is important to me. What's so important about school?
Wednesday, February 27, 2008
My Little Princesses
I never called my twins schizophrenic. I want my daughters to live a life just like everybody else does, with meaning and hope. To me, they are no different.
However to others, they are different.
Evangeline and Esther have to take medication on a daily basis. This is important in controlling the symptoms and eventually reaching the stage of remission whereby the symptoms will be so mild that they can literally lead a more or less normal life, or else they can relapse very fast.
But with Evangeline and Esther’s conditions, it is hard for them to keep up with the daily medications on their own. They tend to forget about it and sometimes even have difficulties in remembering whether they have taken it or not. So I will always keep pillboxes marked with the days of the week so as to help them as well as myself to keep track of medication schedules. This turns out to be useful most of the times.
Not surprisingly, they are uncomfortable with taking medications everyday. Their classmates often laugh at them. They are like labels which mark them as sick, different, abnormal, laughing stocks, weird… All these are too much for them bear. So once in a while they will refuse to take medications. And as a result of poor compliance, symptoms such as delusion and hallucinations resurface again. It is really heart-breaking for me to look at them suffering and find myself could do nothing about it.
Also, medications give them side-effects. The antipsychotic drugs they are taking now cause them to experience drowsiness, restlessness, muscle spasms, weight gain, tremor, dry mouth and blurring of vision. Though the effects reduce after lowering the dosage, but the problem with weight gain is really bad. Evangeline has gained almost 6 kg after one year of taking the drug. I am afraid that this may affect her health by increasing the risk of heart disease or diabetes. There are other health problems which are associated with excessive weight, such as lower back pain, cancer or breathing problems, I have read about in books. So currently, I am looking for suitable alternative drugs which may help to reduce the side-effects on them.
To an outsider, Evangeline and Esther are introverted and withdrawn despite the fact that they seem to enjoy each other’s company. Even though medication has helped to put their symptoms under control, it does not help to improve their social skills. They show a lack of interest in almost everything around them. Having to live in the hospital once in a while and being very much taken care of, they sometimes find difficulties in doing simples things such as boarding a public bus and ordering food. But they are sixteen now, and I am worried about their future if this continues.
In order to improve this condition, I often bring them out on weekends for family activities, like picnic and shopping trips, so as to expose them to the outside world where on one knows about their illness. This makes them to feel just like normal individuals and apparently they enjoy it.
I do not expect Evangeline and Esther to achieve great things in life. As long as they can enjoy life to the fullest, I am happy.
A Brief Introduction To Schizophrenia -- Diagnosis
Diagnosing schizophrenia is difficult as there is no single symptom which is unique to the disorder. There are no tests that can positively identify schizophrenia in a person. Therefore, the diagnosis depends on excluding other causes that may bring about schizophrenia-like symptoms, such as: substance misuse, epilepsy, brain tumours and thyroid dysfunction.
There are two major systems currently used for the diagnosis of schizophrenia, the Diagnostic and Statistic Manual of Mental Disorders and the International Classification of Disease. These classifications have the effect of improving inter-rater reliability but they do not make diagnosis an objective activity.
Diagnostic & Statistical Manual of Mental Disorders (DSM-IV) Criteria for Schizophrenia:
A. Characteristics of Symptoms: two or more of the following, each present for a significant portion of time during a one month period (or less if successfully treated):
Ÿ Delusions
Ÿ Hallucinations
Ÿ Disorganised speech (e.g. frequent derailment or incoherence)
Ÿ Grossly disorganised or catatonic behaviour
Ÿ Negative symptoms, i.e. affective flattening, alogia or avolition
(Note: Only one "A" symptom is required if delusions are bizarre or hallucinations consist of a voice keeping up a running commentary on the person's behaviour or thoughts, or two more voices conversing with each other).
B. Social/Occupational Dysfunction: for a significant portion of time since the onset of the disturbance, one or more major areas of functioning, such as work, interpersonal relations or self-care is markedly below the level achieved prior to the onset (or when the onset is in childhood or adolescence, failure to achieve expected level of interpersonal, academic or occupational achievement).
C. Duration: continuous signs of the disturbance persist for at least six months. This six month period must include at least one month of symptoms that meet criterion A (i.e. active phase symptoms) and may include periods of prodromal or residual symptoms. During these prodromal or residual periods, the signs of disturbance may be manifested by only negative symptoms or two or more symptoms listed in criterion A present in an attenuated form, e.g. odd beliefs, unusual perceptual experiences).
Exclusion Criteria: the remainder of the criteria (D-F in the DSM-IV text) specify that the signs and symptoms above are not better accounted for by another disorder, either psychiatric (i.e. mood disorder, schizoaffective disorder or pervasive developmental disorder), substance abuse (e.g. amphetamine intoxication or withdrawal) or a general medical condition (e.g. hyperthyroidism).
International Classification of Disease (ICD-10) Criteria for Schizophrenia:
Either at least one of the syndromes, symptoms and signs listed below under (1) or at least two of the symptoms and signs listed under (2) would have been present for most of the time during an episode of psychotic illness lasting for at least 1 month.
1. At least one of the following:
Ÿ Thought echo, thought insertion or withdrawal and thought broadcasting.
Ÿ Delusions of control, influence or passivity, clearly referred to body or limb movements or specific thoughts, actions or sensations, and delusional perception.Hallucinatory voices giving a running commentary on the patient's behaviour or discussing him/her between themselves or other types of hallucinatory voices coming from some part of the body.
Ÿ Persistent delusions of other kinds that are culturally inappropriate or implausible, such as religious or political identity, superhuman powers and ability etc.
2. At least two of the following:
Ÿ Persistent hallucinations in any modality, when accompanied by either fleeting or half-formed delusions without clear affective content or by persistent over-valued ideas or when occurring every day for weeks or months on end.
Ÿ Breaks of interpolations in the train of thought, resulting in incoherence or irrelevant speech or neologisms.
Ÿ Catatonic behaviour, such as excitement, posturing or waxy flexibility, negativism, mutism and stupor.
Ÿ Negative symptoms such as marked apathy, paucity of speech and blunting or incongruity of emotional responses (these usually result in social withdrawal and lowering of social performance). It must be clear that these are not due to depression or neuroleptic medication.
Ÿ A significant and consistent change in the overall quality of some aspects of personal behaviour, manifest as loss of interest, aimlessness, idleness, a self-absorbed attitude, and social withdrawal.
Exclusion Criteria: The ICD-10 criteria specify that schizophrenia should not be diagnosed if the symptoms are better accounted for by a mood disorder, 'overt brain disease' or drug intoxication or withdrawal.
References:
Adapted from http://www.sfnsw.org.au/schizophrenia/diagnosis.htm. SFNSW Inc...Locked Bag 5014 Gladesville NSW 1675...ph: 02 9879 2600...fax: 02 9879 2699...Email: admin@sfnsw.org.au
Tuesday, February 26, 2008
A Brief Introduction To Schizophrenia -- Symptoms
By reading through some of the causes of schizophrenia in the causes section, you may have gotten an inkling of the symptoms of the disorder.
So now let us watch a video clip on the common symptoms of schizophrenia. In this clip, some of the way of diagnosis and treatments can also be found.
The symptoms of schizophrenia are often divided into two groups:
Ÿ Positive symptoms: excesses or distortions of normal mental functions, e.g. hallucinations and delusions
Ÿ Negative symptoms: a loss or reduction of normal functioning and are more difficult to evaluate because they may be influenced by a concurrent depression or a dull and unstimulating environment, e.g. apathy and poverty of speech
Positive symptoms
Ÿ Hallucinations: They are often being described by family and friends as a wild imagination. The perceptions are sensory and involve sound, sight, touch and smell. Hearing voices is the most common type of hallucination in schizophrenia patients. The voices may describe the patients' emotions or activities, carry on a conversation, warn of dangers or even tell the patient what to do next.
Ÿ Delusions: People who experience delusions are convinced that their opinions and beliefs are real, despite evidence to the contrary. About one third of patients suffer from paranoid-type symptoms and often have delusions of persecution or suffer from irrational beliefs that they are being cheated, harassed, poisoned, or conspired against.
Ÿ Disorganised thinking: Schizophrenia often affects a person's ability to think straight. Thoughts may flash by; concentration is difficult and the patient is often easily distracted, unable to focus his/her attention. People with schizophrenia often find it difficult to decide what is or is not relevant to a situation. They are unable to connect thoughts into logical sequences and their thoughts become disorganised and fragmented. This lack of logical thought process, called thought disorder, can make a conversation very difficult and result in social isolation.
Ÿ Agitation: Schizophrenia patients are often extremely agitated.
Negative symptoms
Ÿ Lack of drive or initiative: A distinct lack of drive or initiative is often observed in patients. They seem to have lost their enthusiasm or interest in things.
Ÿ Social withdrawal: People with schizophrenia tend to become isolated and often prefer their own company and avoid contact with others. When forced to interact, they often have nothing to say.
Ÿ Apathy: Often people with schizophrenia appear totally indifferent to their surroundings and are not interested in taking part in things. Motivation can decrease significantly, as can interest in or enjoyment of life. In severe cases, a person can spend entire days doing nothing at all, even neglecting basic hygiene.
Ÿ Emotional: unresponsiveness or blunting People with schizophrenia often display blunted or flat emotions. They suffer from severely reduced emotional expression and may not be able to show normal emotions. For example, they may speak in a monotonous voice, show little facial expression and appear extremely indifferent.
Reference:
Janssen Pharmaceutica, NV - Turnhoutseweg 30, 2340 Beerse, Turnhout RPR nr.0403.834.160 © Janssen Pharmaceutica, NV 2008 Last updated on 26 Jul 2007 http://www.janssen-cilag.com/
Monday, February 25, 2008
I'm excited for this is my first time!
A Brief Introduction To Schizophrenia -- Causes
Possible Causes
Before we start to talk about schizophrenia, this video clip below may help to provide you with some general ideas about this disorder. So sit back and enjoy!
The causes of mental illness are linked to several factors which can be summarised into three main groups:
Ÿ Biological factors which arise from physiology, biochemistry, genetic make-up and physical constitution
Ÿ Psychological factors including the person's upbringing, emotional experiences and interactions with people
Ÿ Social factors that are associated with the person's present life situation and socio-cultural influences
However, no single cause can account for schizophrenia. Rather, it appears to be the result of multiple "hits". Here we will focus on some of the biological factors.
Abnormalities in Brain Structure, Circuitry, and Chemicals
Brain scans using magnetic resonance imaging (MRI) have shown that there are a number of abnormalities in the brain's structure associated with schizophrenia. Such abnormalities can cause nerve damage and disconnections in the pathways that carry brain chemicals.
1. Abnormal Brain Activity and Volume.
Imaging techniques have revealed abnormal brain activity and shrinkage (reduced volume) in the brains of people with schizophrenia. Of particular importance are those in the prefrontal cortex , which contains the white matter of the brain, and the temporal lobes , which contain the limbic system.
Shrinkage of the prefrontal cortex can damage nerve cells and impair the connections that are required for verbal memory, attention, decision-making, reasoning, aggression, and meaningful speech. Impairment in the left side of the cortex is also associated with auditory hallucinations (hearing voices).
Shrinkage in the limbic areas of the brain is associated with problems finding words. The limbic areas of the brain contain the hypothalamus (controls physiological functions), amygdala (responsible for arousal and emotional states), and hippocampus (the part of the brain that makes memories). A number of studies have specifically noted smaller left hippocampi in people with schizophrenia.
2. Abnormal Brain Chemicals.
Schizophrenia is associated with an unusual imbalance of neurotransmitters (chemical messengers between nerve cells) and other factors.
Abnormal Circuitry
Abnormalities in brain structure are also reflected in the disrupted connections between nerve cells that are observed in schizophrenia. Such miswiring could impair information processing and coordination of mental functions. For example, auditory hallucinations may be due to miswiring in the circuits that govern speech processing. Strong evidence suggests that schizophrenia involves decreased communication between the left and right sides of the brain.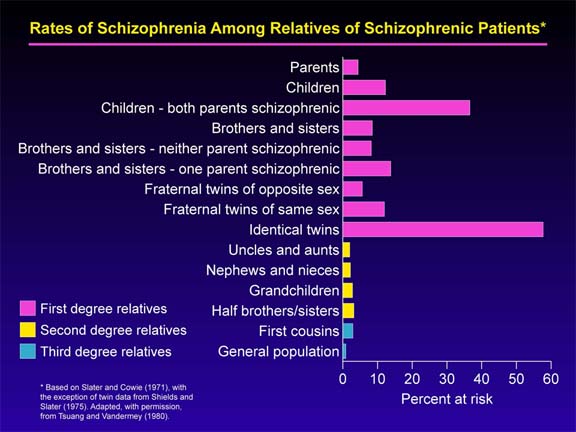
Genetic Factors
Schizophrenia undoubtedly has a genetic component. (refer to graph on the right for clearer view) Current evidence suggests that there are a multitude of genetic abnormalities involved in schizophrenia, possibly originating from one or two changes in genetic expression. Scientists are beginning to discover the ways in which specific genes affect particular brain functions and cause specific symptoms.
Infectious Factors
The case for viruses as a cause of schizophrenia rests mainly on circumstantial evidence, such as living in crowded conditions. The risk is higher for people who are born in cities than in the country. The longer one lives in the city, the higher the risk. The following are some studies suggesting an association:
Ÿ Winter and Spring Births: The risk for schizophrenia worldwide is 5 - 8% higher when colds and viruses are more prevalent.
Ÿ Large Families: The risk for schizophrenia is also greater in large families in which there are short intervals between siblings (2 or fewer years). Such observations suggest that exposure to infection early in infancy may help set the stage for later development of the disease.
Ÿ Pregnant Mother's Exposure to Viruses: The mother's exposure to viral infections such as rubella, measles, chicken pox, or others while the infant is in the womb has also been associated with higher risk for schizophrenia in her child.
Loss of Oxygen around the Time of Birth
Many studies have reported an association between schizophrenia and problems surrounding birth, particularly those that cause oxygen deprivation, which could affect the nerve growth or structure in the developing brain. Specific complications that have been associated with such a higher risk include:
Ÿ Prolonged labor
Ÿ Bleeding during pregnancy
Ÿ A short gestation period and low birth weight
Psychological Factors
Although parental influence is no longer believed to play a major role in the development of schizophrenia, it would be irresponsible to ignore outside pressures and influences that may exacerbate or trigger symptoms. The prefrontal lobes of the brain, which are the brain areas often thought to lead to this disease, are extremely responsive to environmental stress. Given the fact that schizophrenic symptoms naturally elicit negative responses from the patient's circle of family and acquaintances, it is safe to assume that negative feedback can intensify deficits in a vulnerable brain and perhaps even trigger and exacerbate existing symptoms.
References
Information taken from http://health.nytimes.com/health/guides/disease/schizophrenia/print.html
Life Is Not Always In Sunshine
Up to this point you may think: “What a happy life this woman has!” Indeed, God seems to be too good to me: a smooth career, a caring husband and most importantly, three healthy daughters. But just like what Virgil says: “Life is not always in sunshine.” I only come to appreciate what this classical Roman poet says when I discovered two years ago that both Evangeline and Esther are schizophrenic.
The first sign of their illness appeared when we were watching TV in the living room one Sunday afternoon. Esther started to say something like people on television are aiming special messages at her and that her thoughts are being broadcast aloud to others.” I did not take this seriously at first. But her strange behaviours carried on for a few days whereby she became agitated easily at trivial matters and insisted that everyone was conspiring against her. Teachers at her school complained about her inabilities to concentrate in class and the tendency to stay away from other kids. So that was when I started to become worried and I brought her to the doctor straight away.
So at the psychiatry department, I was being asked to recount Esther's recent behaviours and family medical history as Esther for no reason refused to talk to him. As I faithfully answered each and every one of his questions, something ominous struck my mind: my grandfather was schizophrenic!
After that, Esther went through various blood test, urine test, special IQ tests, etc, which really scared me. The results come out that what was troubling Esther all these day was indeed schizophrenia, an undifferentiated type and chronic.
I was devastated. For a few days I could not believe the fact. So I went on to surf the net, hoping that someone out there would have something the opposite to say. I was disappointed and this disappointment became a fear when I came across this video clip while I was researching.
Was this what my little Esther was experiencing right now? All the inner voices and hallucinations and all. I hoped that I could be the one that was suffering all these.
However, misfortunes never come singly.
Maybe it is the kind of mutual affinity and attachment that always exist between twins, half a year later, Evangeline was being diagnosed of schizophrenia as well. Actually I was mentally prepared for this as the doctor which Esther went to had already warned me of this possibility. I told myself it was time to get over my misery. It is unfortunate of my little twins to suffer from such illness before they could have a chance to enjoy all the wonders in life, but I, being their mother, should brace up and make the best out of whatever life has bestowed on them.
Sunday, February 24, 2008
A Brief Introduction To Schizophrenia
 Schizophrenia is a chronic, severe, and disabling brain disorder that has been recognized throughout recorded history. It is found all over the world, in all races, in all cultures and in all social classes, and it affects 1 in 100 people worldwide. It is probably one of the most common brain disorders in the world (refer to chart on the right) and both men and women are affected with equal frequency though for men, the age of onset is often between16 and 20, whereas for women, it is sometimes later -- ages 20 to 30.
Schizophrenia is a chronic, severe, and disabling brain disorder that has been recognized throughout recorded history. It is found all over the world, in all races, in all cultures and in all social classes, and it affects 1 in 100 people worldwide. It is probably one of the most common brain disorders in the world (refer to chart on the right) and both men and women are affected with equal frequency though for men, the age of onset is often between16 and 20, whereas for women, it is sometimes later -- ages 20 to 30.